How to maintain a healthy gums or gingiva?
First of all, Maintaining a healthy gums is essential for good oral hygiene and overall dental health. Gum disease, also known as periodontal disease, is a common condition that affects millions of people worldwide. However, by following a few simple practices, you can prevent gum disease and keep your gums healthy.
Introduction
The gingiva, also known as the gums, is the pink-colored mucosa that surrounds and protects the teeth.
The gum or gingiva is part of the periodontium, which includes the investing and supporting structures of the teeth.
Additionally, signs of systemic disease frequently manifest in the mouth, and poor oral gums health can worsen many systemic conditions.
The gums epithelium (thin tissue) plays a crucial role in the innate immune response to infectious inflammation in periodontal tissue. Thus, it is a key mediator in the initiation of periodontal disease.

GINGIVAL AND PERIODONTAL DISEASES
1. GINGIVITIS
Gingivitis is defined as a reversible plaque-induced ( tartar) inflammation limited to the gingiva.
Clinical signs and diagnostic methods
Gingivitis manifests clinically as swelling, reddening and bleeding of the gingival margin , accompanied by halitosis ( bad breath) . It is diagnosed clinically by means of a combination of visual inspection and tactile examination. The presence and degree of gingival inflammation is assessed based on a combination of redness and swelling, as well as presence or absence of bleeding on gentle probing of the gingival sulcus.
Treatment-
- Scaling and polishing in every 6 months.
- Using of mouth wash like chlorhexidine 0.12 % (antiplaque),
- Proper brushing twice a day.

2. PERIODONTAL DISEASE-
Periodontal disease is a general term that refers to all diseases involving the supporting structures of the teeth (periodontium), including the gingiva, periodontal ligament, alveolar bone, and cementum. In the early phase of periodontal disease, infection is confined to the gingiva (gingivitis).
Later, the underlying supporting tissues are affected (periodontitis), ultimately leading to complete destruction of the periodontium and a permanent loss of teeth.
Periodontal infections tend to localize in intraoral soft tissues and seldom spread into deeper structures of the face or neck.
The gingiva is inflamed and discolored, bleeds readily, and appears as periodontal pockets around the affected teeth.
Frank pus can be readily expressed by digital pressure, or it may exude freely from the pockets. As periodontitis advances, the supporting tissues are destroyed, ultimately leading to loosening and exfoliation of teeth.
Periodontitis is subdivided into:
- Chronic periodontitis: the main type of periodontal disease characterized by slow destruction of the periodontal tissues.
- Aggressive periodontitis: periodontitis showing rapid periodontal breakdown, considered not to be equivalent with the level of plaque present.
- This unusual but severe type of periodontitis is typically seen in adolescents and young adults (< 35 years old), and can occur in localized (restricted to first molars and incisors) and generalized (affecting at least two other teeth) forms.

3. PERIODONTAL ABSCESS
Periodontal abscesses may be focal or diffuse and manifest as red, fluctuant swelling of the gingiva, which is extremely tender to palpation. These abscesses are always in communication with a periodontal pocket from which pus can be readily expressed after probing. Commonly occur in uncontrolled diabetic patients.
Treatment –
It has surgical and aimed at drainage of loculated pus. After abscess resolution, endodontic or periodontal infections should continue to be treated by removal of necrotic infected pulpal tissues or by subgingival scaling and root planing.
Apical surgery may sometimes be necessary to reach the apical part of the root for débridement.

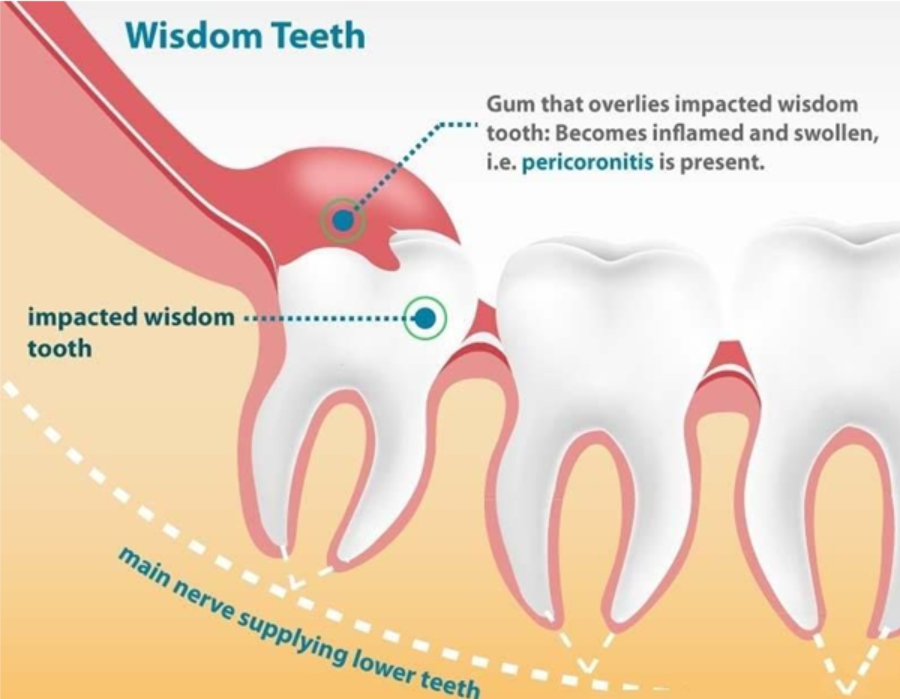
4. PERICORONITIS
Pericoronitis is an acute localized infection associated with gum flaps overlying a partially erupted or impacted wisdom tooth ( 3rd molar).
Food debris and microorganisms become entrapped under the affected gingival tissues. If drainage is interrupted by sudden swelling or trauma, infection extends along fascial planes of least resistance into adjacent soft tissues. The underlying alveolar bone is usually not involved.
Clinically, the pericoronal tissues are erythematous and swollen. Digital pressure produces a small amount of exudate from under the infected flap. Because the masticator spaces are often involved, marked trismus (restricted mouth opening) secondary to irritation of the masseter or medial pterygoid muscle is a prominent presenting feature.
Treatment-
Includes incision of the lesion and irrigation of the pericoronitis pouch with antiseptics.
Systemic antibiotics may be necessary if cellulitis of fascial planes occurs. Excision of the operculum or extraction (in case of 3rd molar) of the involved tooth may also be considered.
Treatments –
- Emergency phase – extraction of hopeless teeth ( grade 3 mobility of tooth) .
- Non – surgical phase – removal of calculus and root planning , restoration of caries tooth.
- Surgical phase – periodontal therapy ( grafting ), endodontic therapy ( root canal treatment) , Implants.
- Restorative phase – fixed and removable prosthetics ( denture ).
- Maintenance phase – re-checking every 6 months .